Background: The incidence of both myeloid malignancies and cardiovascular disease (CVD) increases with age, and cardiac disease is the most frequent cause of non-hematologic morbidity in patients with myelodysplastic syndrome (MDS). We aimed to study whether the presence of CVD is associated with worse outcomes in patients with myeloid malignancies.
Methods: We retrospectively reviewed 295 patients diagnosed with acute myeloid leukemia (AML), MDS or MDS/myeloproliferative neoplasm (MDS/MPN). CVD included congestive heart failure (CHF), coronary artery disease (CAD), arrhythmia, peripheral vascular disease, congenital heart disease and/or cerebrovascular accident. Endpoints included overall response rate (ORR), overall survival (OS), cardiac events and death within 60 days of treatment initiation. Patient characteristics were compared between those with CVD vs. no-CVD using the Fisher's exact and t-tests. The Kaplan-Meier approach was used to estimate OS. The multivariate Cox regression model was utilized to identify predictors of OS.
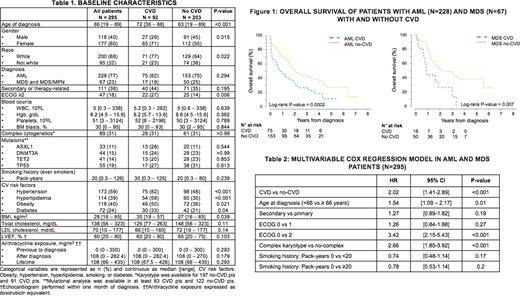
Results: Patient characteristics are summarized in Table 1. The study population included 92 patients (31%) with CVD and 203 (69%) without CVD, with a median age of 66 years (range 19-89) at diagnosis. Patients with CVD were older (p <0.001) and had higher rates of hypertension (p <0.001), hyperlipidemia (p<0.001), diabetes (p=0.04) and obesity (p=0.02) (Table 1). Treatment was hypomethylating agent (HMA)-based, anthracycline-based or other in 78%, 20% and 2% of CVD patients, compared to 56%, 41% and 3%, respectively, in no-CVD patients (p=0.001).
Among the 228 AML patients, 20% vs. 48% of patients in the CVD vs. no-CVD groups achieved complete remission (CR), 24% vs. 22% achieved CR with incomplete count recovery (CRi), 1% vs. 3% achieved partial remission (PR), 20% vs. 17% were primary refractory (p <0.001), and 33.3% vs. 10.5% had early death. Among the 67 MDS and MDS/MPN patients (grouped as MDS), 12% vs. 6% CVD vs. no-CVD patients achieved CR, 6% vs. 0 CVD patients achieved CRi; 6% vs. 16% achieved hematologic improvement (HI); 0 vs. 2% of no-CVD patients achieved PR; and 12% vs. 4% had early death (p= 0.04).
For AML patients, 1-, 2- and 3-year OS in CVD vs. no-CVD groups (Figure 1) was 46% vs. 70%; 34% vs. 53%; and 26% vs. 43%, respectively [HR 1.9, 95% CI = 1.35, 2.67]. For MDS patients it was 44% vs. 81%, 26% vs. 51%, and 26% vs. 49%, respectively [HR 2.52, 95% CI = 1.27, 5]. In a multivariable regression model accounting for age, performance status and karyotype, CVD was an independent prognostic factor for worse OS (Table 2). Smoking history (pack-years) did not impact OS. There was a trend toward fewer CVD than no-CVD patients undergoing allogeneic transplantation (17.4% vs. 27.6%, p=0.08). With a median follow-up of 15 months in both groups, 75% of AML and MDS patients with CVD were deceased, compared to 54% of no-CVD patients (p <0.0001).
Cardiac adverse events were more frequent in CVD compared to no-CVD patients, including myocardial infarction/demand ischemia (13% vs 2%, p= 0.0003), arrhythmia (20% vs 10%, p= 0.01), and CHF exacerbations (27% vs 10%, p= 0.002).
Conclusions: Our study demonstrated that presence of CVD is a very important predictor of survival outcomes of patients with AML and MDS. As the incidence of both CVD and myeloid malignancies increases with age, a better understanding of their association and shared complications can translate into better therapeutic options.
Emadi:Amgen: Membership on an entity's Board of Directors or advisory committees; Genentech: Membership on an entity's Board of Directors or advisory committees; Jazz Pharmaceuticals: Research Funding; Servier: Membership on an entity's Board of Directors or advisory committees; KinaRx: Other: co-founder and scientific advisor; NewLink Genetics: Research Funding. Baer:Astellas: Other: Institutional research funding; AbbVie: Other: Institutional research funding; Incyte: Other: Institutional research funding; Forma: Other: Institutional research funding; Takeda: Other: Institutional research funding; Kite: Other: Institutional research funding; Oscotec: Other: Institutional research funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal